Fluoroscopy is one of the most important technologies in modern medical imaging, allowing doctors and specialists to view internal body structures in real-time. This revolutionary technique has transformed diagnostic methods and interventional procedures in medicine, significantly improving diagnostic accuracy and guiding treatments more effectively. In this detailed article, we will explore the working mechanism of this technique, its applications, benefits, associated risks, and the latest advancements in this vital field of medical engineering.
What is Fluoroscopy?
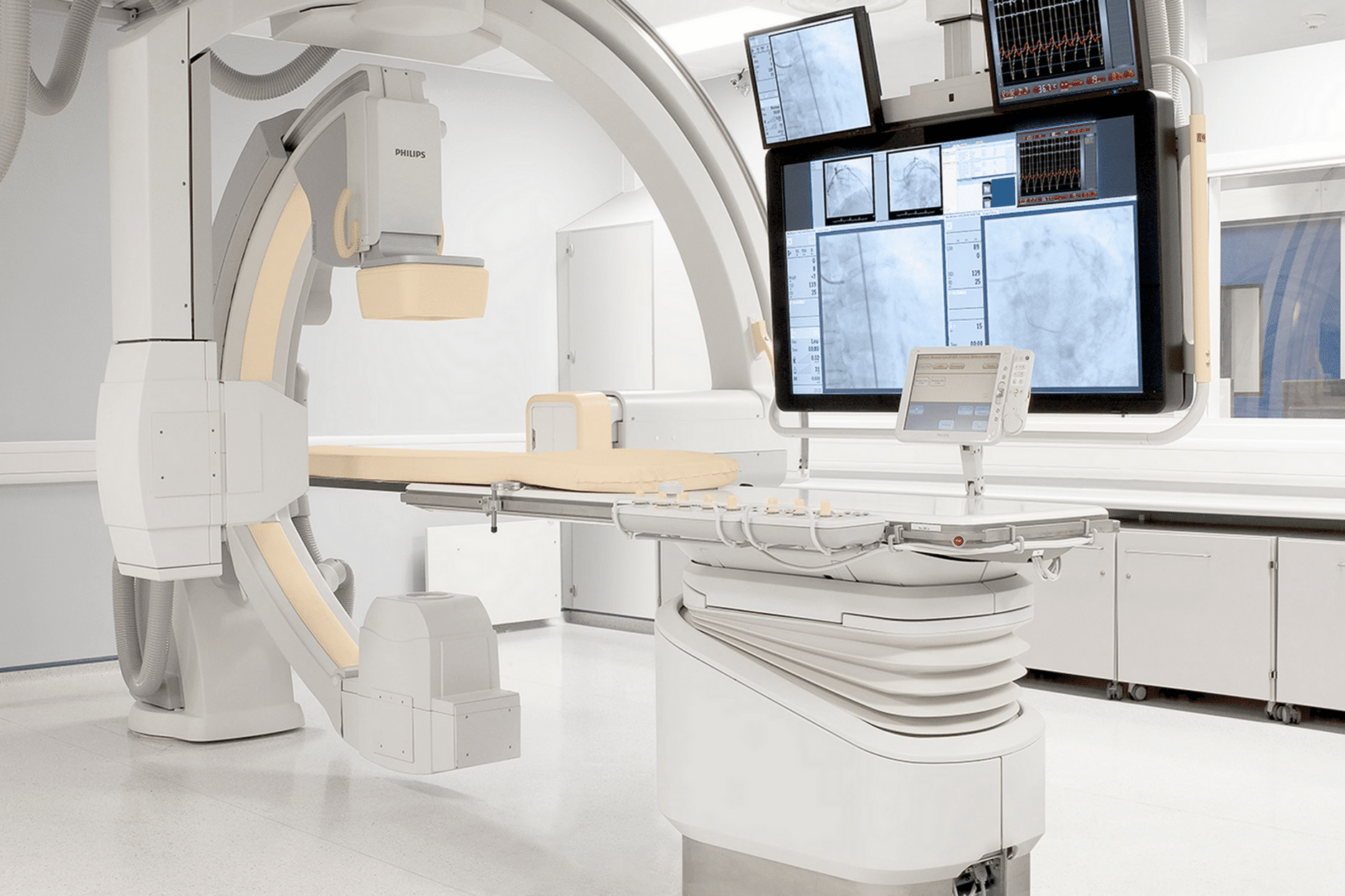
Fluoroscopy is an advanced imaging technique that utilizes X-rays to generate a continuous series of images displayed as a real-time video. This technique is widely used in emergency departments, operating rooms, and diagnostic radiology clinics, enabling surgeons and physicians to monitor the movement of organs and internal structures during procedures or diagnostic examinations. The increasing reliance on fluoroscopy reflects its significance in providing accurate and immediate insights into various medical conditions.

Fundamental Principles of Fluoroscopy
Fluoroscopy is extensively used across multiple medical specialties, enhancing the quality of healthcare. To fully understand this technique, it is essential to delve into the fundamental principles that underpin fluoroscopy, forming its scientific and technical foundation.
X-ray Mechanism
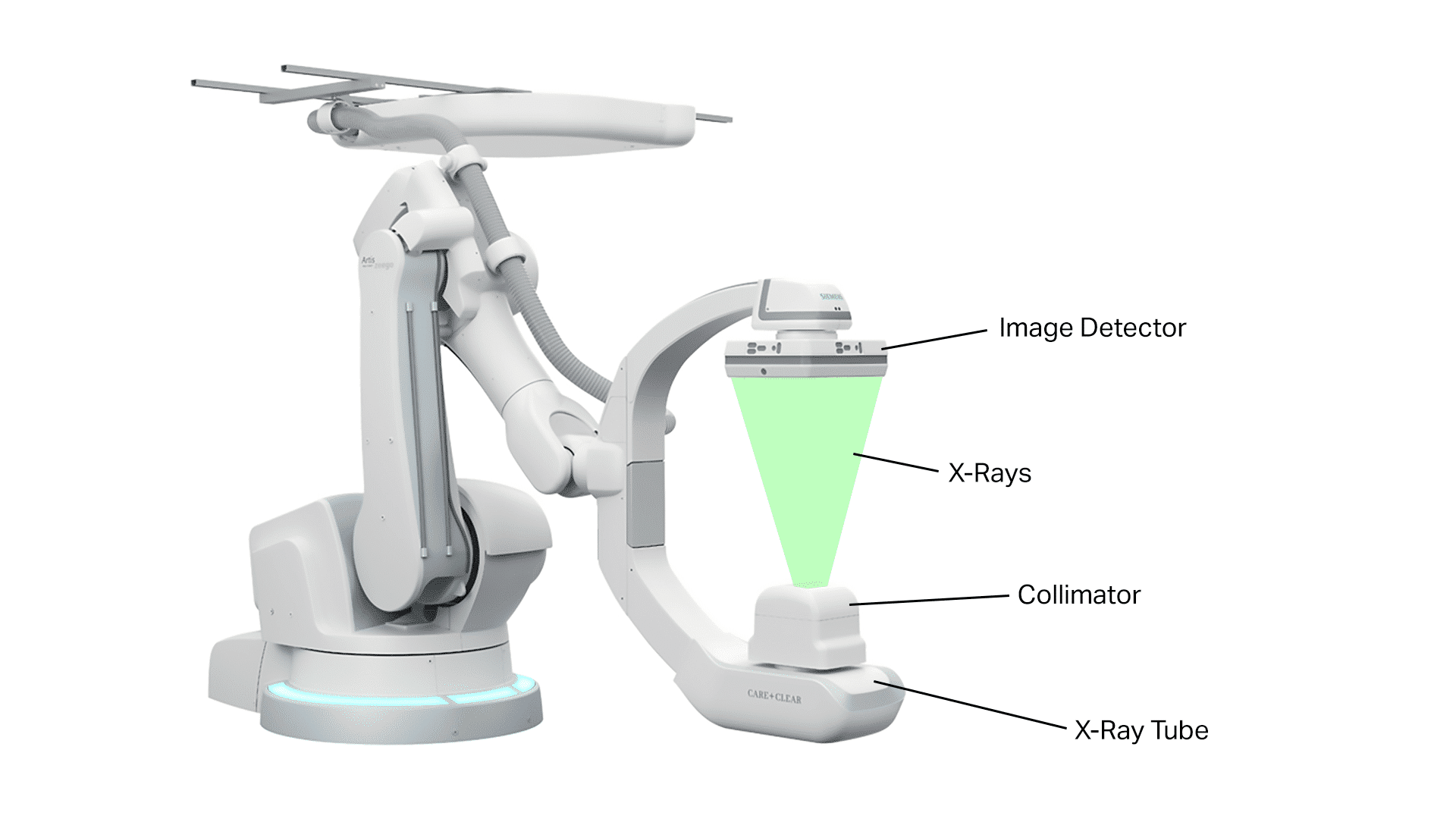
This technique operates on the same principles as conventional X-ray imaging but with the ability to produce sequential images in real time, creating a video-like sequence of still images. The process begins with generating X-rays through a specialized tube, where a high-voltage current is applied. This accelerates electrons toward a metallic target, typically tungsten—a chemical element. Upon collision, X-rays are emitted and directed toward the area of the body being examined.
Image Intensification
The image intensifier in fluoroscopy plays a crucial role in enhancing the clarity of internal details. This device amplifies the signals produced by X-rays passing through the body, resulting in a bright and clear image. Recent advancements have led to the replacement of traditional image intensifiers with flat-panel detectors, which provide high-quality images while minimizing radiation exposure.
Diverse applications of Fluoroscopy
Fluoroscopy has a wide range of medical applications, both in diagnostics and interventional procedures. This system is highly flexible and capable of providing real-time moving images, allowing doctors to monitor physiological changes instantly.

Diagnostic Applications
Fluoroscopy is used in several essential diagnostic procedures, including:
- Gastrointestinal Studies: Fluoroscopy is employed to assess the digestive tract, including the esophagus, stomach, and intestines. Barium studies, such as barium swallow and barium enema, help evaluate abnormalities or motility disorders.
- Neuromuscular and Spinal Imaging: This technique is used in diagnostic imaging of the spine, particularly in myelography, which aids in assessing spinal cord conditions.
- Joint Evaluations: For joint-related issues, fluoroscopy is also used in arthrography to evaluate abnormalities or injuries affecting the joints.
Interventional Applications
This technique is a cornerstone in medical engineering for interventional procedures, providing live imaging during operations, which contributes to:
- Guiding Surgical Procedures: Fluoroscopy assists in catheter placement during cardiac procedures, such as coronary angiography, ensuring precise positioning and minimizing procedural risks.
- Interventional Treatments: It is utilized in therapeutic interventions, including stent placement, bone fixation in fracture surgeries, and the insertion of delicate medical devices.
- Minimally Invasive Procedures: This technology facilitates minimally invasive procedures requiring small or no surgical incisions, reducing patient discomfort and promoting faster recovery.
Benefits of Fluoroscopy in Medical Practice
Fluoroscopy is a pioneering technique that enhances medical care quality for several key reasons:
1) Enhanced and Accurate Diagnosis
This technology provides dynamic imaging that reveals the functional movements of internal organs, such as diaphragm motion, intestinal activity, and blood flow through vessels. This capability helps in early disease detection, as moving images can uncover functional changes that static images might not reveal.

2) High Precision in Interventional Procedures
By offering live imaging during medical procedures, fluoroscopy enables precise manipulation of medical instruments within the body. This reduces the likelihood of surgical complications and improves success rates in procedures like stent placement and fracture fixation.
3) Reduced Surgical Invasiveness
This technique allows for numerous minimally invasive procedures, reducing the need for major surgeries. Minimally invasive techniques are less painful, promote faster recovery, and lower the risk of post-operative infections, making them a significant advancement in modern medicine.
Risks and Safety Considerations in Fluoroscopy
Despite the significant benefits of fluoroscopy, there are certain risks associated with its use that must be carefully considered.
Radiation Exposure
Radiation exposure is one of the primary concerns when using fluoroscopy. Prolonged procedures may increase the amount of radiation a patient is exposed to. The level of exposure depends on the duration of the procedure and the examined area. To mitigate these risks, advanced techniques such as pulsed fluoroscopy and dose-reduction algorithms have been developed to minimize radiation exposure.
Contrast Media Reactions
Contrast media are often used during this technique to enhance the visibility of internal structures. However, some patients may have allergic reactions to these substances, ranging from mild skin rashes to severe anaphylactic responses. To manage these risks, pre-procedure screening and emergency medications are utilized when necessary.
Occupational Radiation Exposure
Medical professionals performing frequent fluoroscopy procedures are at risk of occupational radiation exposure. Strict protective measures, such as wearing personal protective equipment (e.g., lead aprons and thyroid shields), are essential. Additionally, regular monitoring of radiation levels ensures the safety of doctors and healthcare staff, helping to prevent potential long-term risks.
Recent Advances in Fluoroscopy Technology
The field of fluoroscopy has seen significant advancements in recent years, leading to improved image quality and reduced radiation risks. Traditional systems have been replaced with digital fluoroscopy using flat-panel detectors, which enhance image resolution while minimizing radiation exposure. This digital system provides high-definition images and allows for post-processing adjustments to refine diagnostics. Additionally, it enables seamless image sharing among medical teams for quick consultations and decision-making.
Furthermore, the integration of cone-beam computed tomography (CBCT) with fluoroscopy now offers detailed 3D imaging for complex anatomical assessments. This technology is widely used in dentistry, orthopedic surgeries, and interventional procedures requiring precise localization.
Moreover, combining this technique with other imaging modalities such as ultrasound and magnetic resonance imaging (MRI) has led to the development of hybrid imaging systems. These systems provide both anatomical and functional insights, enhancing diagnostic accuracy and guiding interventional procedures more effectively, particularly in oncology and tumor treatments.
The Future of Fluoroscopy
The future of this technique looks promising, with continuous research and technological advancements aimed at improving procedural efficiency and reducing radiation-related risks.
Integration of Artificial Intelligence
Artificial intelligence (AI) is expected to play a pivotal role in fluoroscopy’s evolution. AI algorithms can analyze real-time images, detecting anomalies that may be overlooked by the human eye. Additionally, AI-driven techniques can optimize radiation dose reduction strategies, enhancing patient and healthcare worker safety.
Portable Fluoroscopy Systems
Research and development efforts are currently focused on creating portable fluoroscopy units that can be easily transported to emergency departments or remote areas. These mobile units will enable rapid diagnostic imaging and treatment in locations with limited medical infrastructure, thereby expanding access to essential healthcare services.
Exploring Radiation-Free Alternatives
Scientists are actively exploring non-ionizing imaging alternatives such as optical coherence tomography (OCT) and photoacoustic imaging. While these alternatives are still in experimental stages, they hold great potential for reducing radiation-related risks in this technique, potentially revolutionizing the future of medical imaging.
In conclusion, we live in an era where cutting-edge fluoroscopy technologies are transforming medical diagnostics and interventions. However, behind every advanced imaging system stands a well-trained professional who makes critical decisions. This is where HSI Healthcare Training & Consultancy comes in. Join HSI today—not just to keep up with medical advancements, but to lead them. Because in the world of healthcare, history is not just written by machines but by those who master their language. Are you ready to shape the future of medical imaging?
Source: Real-Time Imaging and Its Impact on Modern Medicine